1601006102 : GM Long Case
CASE OF A 65 YR OLD MALE WITH CKD : LONG CASE GM (1601006102)
CASE OF A 65 YR OLD MALE WITH CKD : LONG CASE GM FINALS
1601006102
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This is the case i have been given :
A 65 year old male who was a farmer came to the OPD with
CHIEF COMPLAINTS OF :
1. Decreased urine out since 4 months
2. Bilateral pedal edema since 4 months and
3. Abdominal distension since 4 months
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 4 months back then developed decreased urine output , which is insidious in onset with decreased frequency and later facial puffiness followed by bilateral pedal edema , pitting type, gradually progressed to involve abdomen with abdominal distension he was admitted to the local hospital where he was diagnosed as acute kidney injury , no aggregating and relieving factors.
There is history of pruritus and pigmentation of both the lower limbs
PAST HISTORY :
He was k/c/o HTN since 5 yrs and was on medications
No h/o suggesting DM, CAD, CVA, TB, asthma, epilepsy
10 yrs back patient had a road Traffic accident for which surgery(? Intramedullary nail insitu) was done for ?hip fracture In nalgonda govt hospital. He had taken NSAIDS for 1 year then.
1 year back patient gives history of taking NSAIDS 3 tabs per day daily for bilateral knee and back pain given by RMP. He took it daily for 1 year
Patient also gives a h/o bilateral Tympanic membrane perforation 6 yrs back (following an infection).
He gives a history of cataract surgery for right eye 10years ago
FAMILY HISTORY :
No k/c/o HTN,DM,TB, asthama,CAD, epilepsy and CKD
PERSONAL HISTORY :
Mixed diet
Appetite is reduced
Sleep is adequate
Bowel regular
Oliguria since 4 months
Addictions : h/o beedi smoking 4-5 years ,stopped 1 year back
GENERAL EXAMINATION :
• Patient is conscious, coherent & cooperative
• Thin built and malnourished
GENERAL SIGNS :
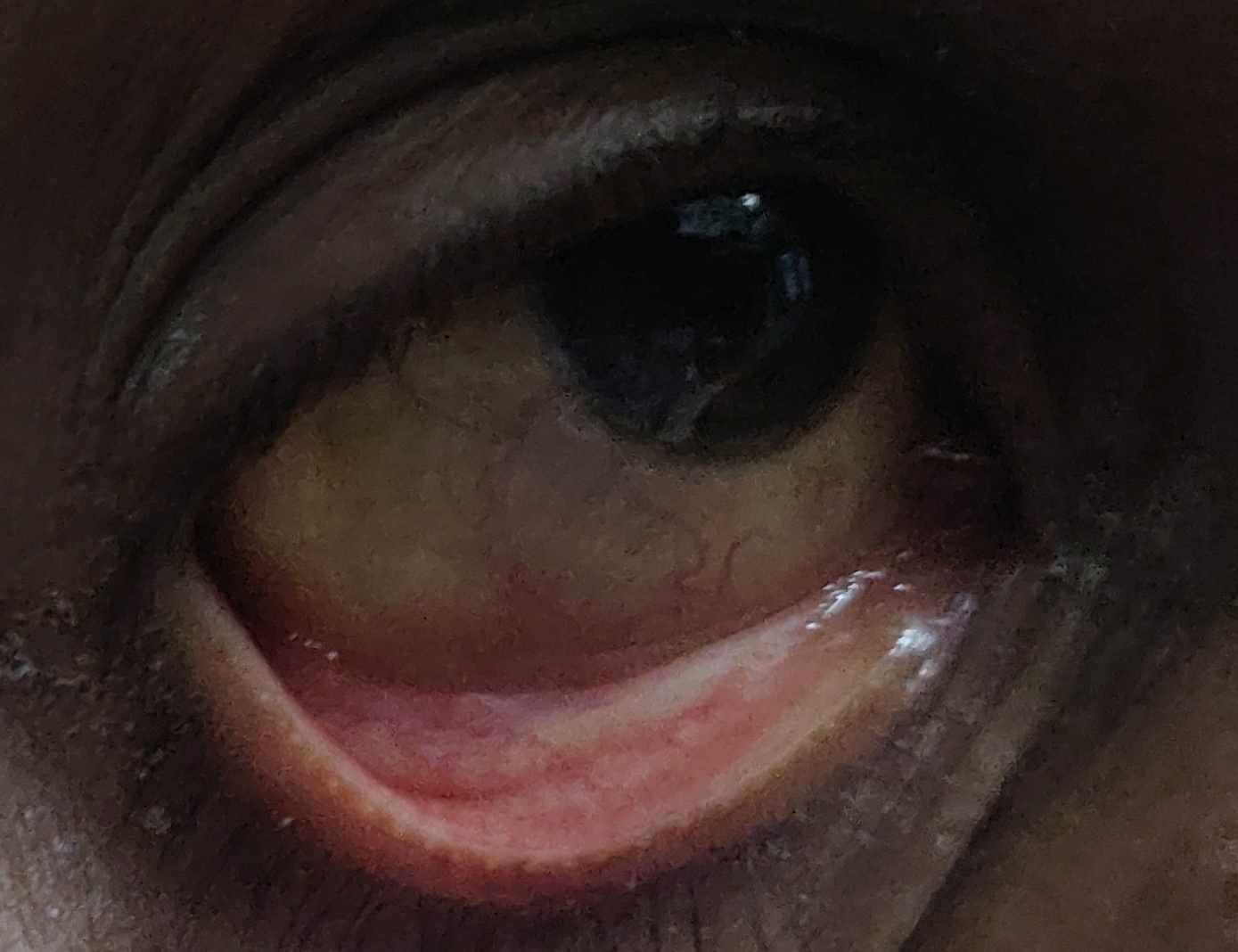
• PALLOR present
PEDAL EDEMA + , which is pitting type
VITALS :
• Temp: 98.5 F,
• RR : 18 cycles/min,
• BP : 100/70mmHg,
• PR : 80/min, regular rythm, normal volume,no radio-radial or radio-femoral delay, Condition of the vessel wall is normal
• SpO2: 97% on RA
SYSTEMIC EXAMINATION :
• CVS: s1 s2 +
no murmurs
• RS:
Bilateral air entry present
Normal vesicular breath sounds, No added sounds
• CNS:
All higher motor functions are normal
Except 8th nerve (Bilateral sensory neural hearing loss present). All other Cranial nerves are intact
Sensory system normal
Motor system normal
Cerebellar signs normal
No meningeal signs
• Per abdomen :
Soft
Non tender
No organomegaly
Bowel sounds heard
INVESTIGATIONS :
Complete blood picture
Complete urine examination
Serum ironRenal function tests
Liver function tests



















Comments
Post a Comment